Two-process model
- Sleep pressure (adenosine): builds while awake; caffeine blocks its receptors temporarily.
- Circadian rhythm: your body clock creates a “sleep gate” at your usual time; morning light advances, late light delays.

Better sleep is a skill. This page shows how sleep works, why insomnia sticks, and the small, repeatable tools — including CBT-I, 3 am rescue steps, and guides for shift work, teens, menopause, pain, PTSD/nightmares, and sleep apnoea.
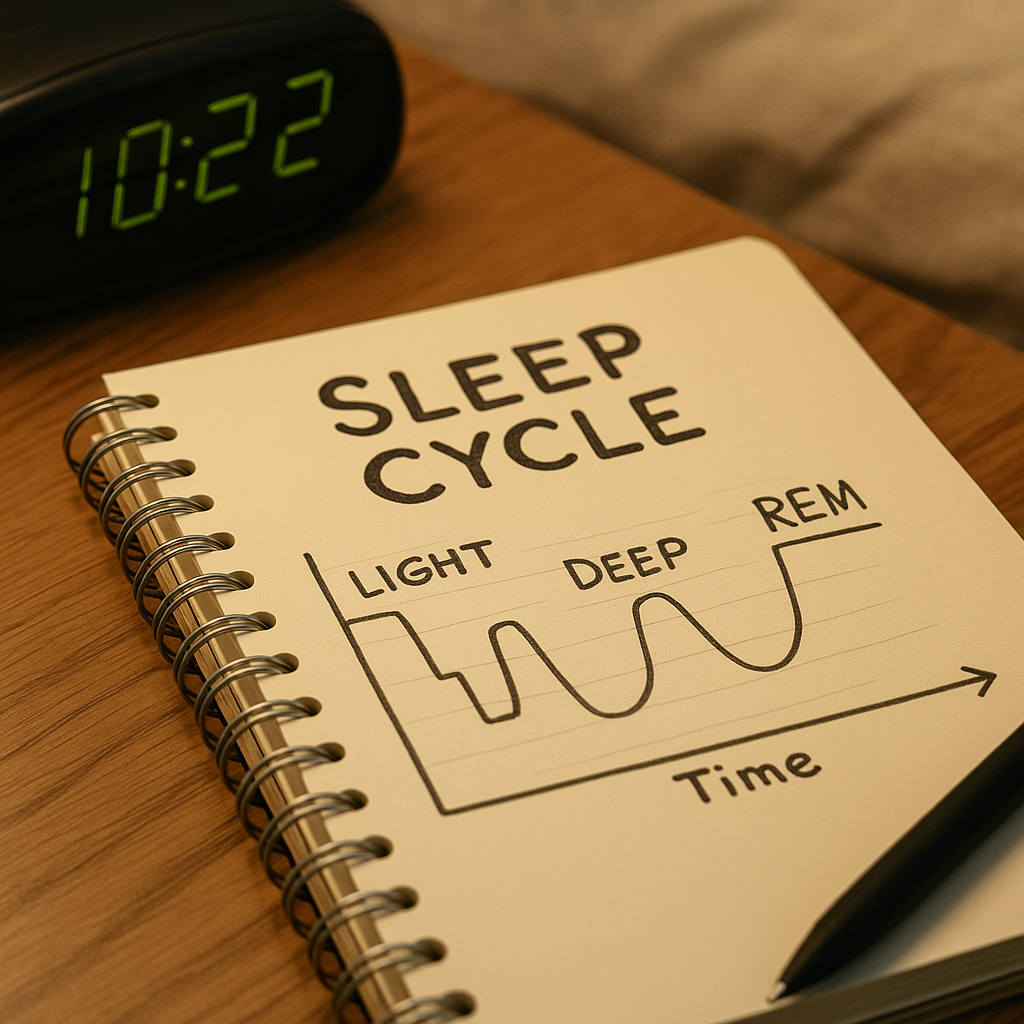
You cycle roughly every 90 minutes: N1 → N2 → N3 (deep) → REM. Later cycles contain more REM.
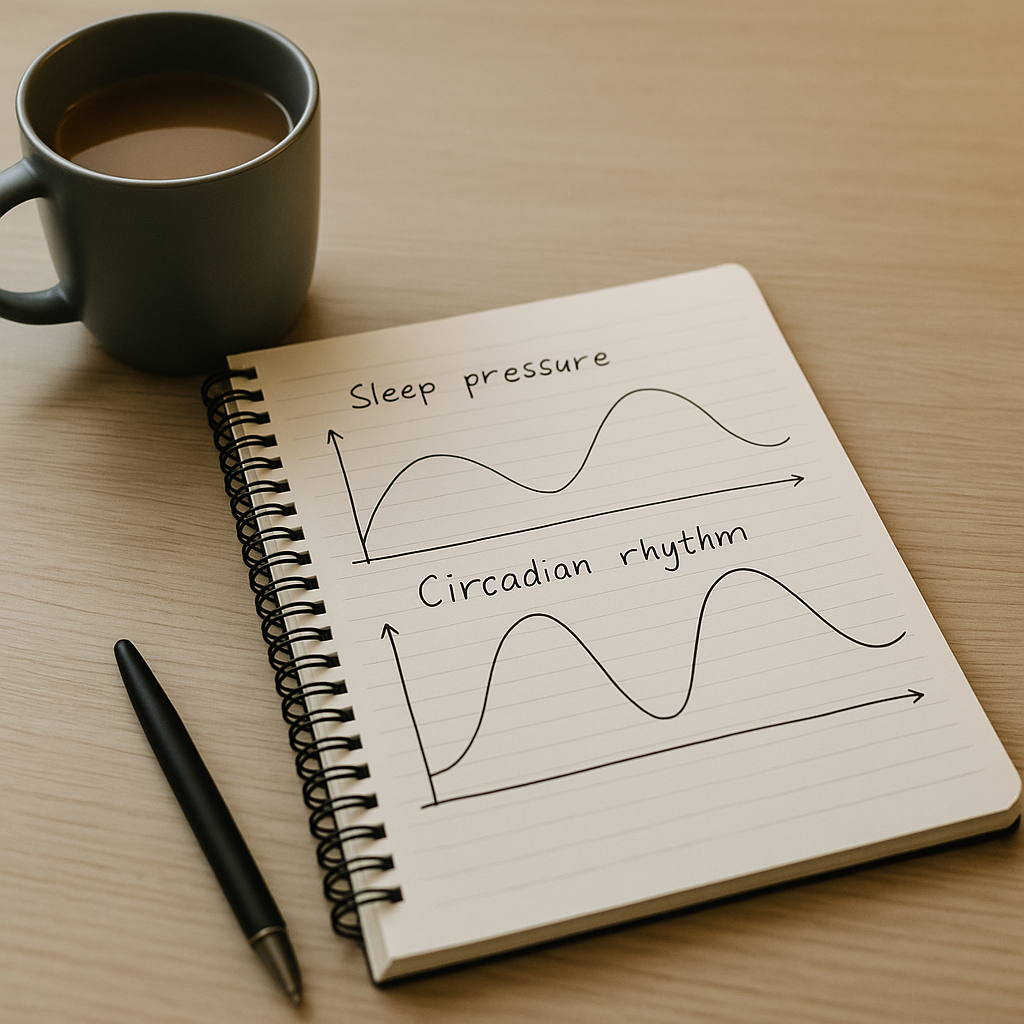
Aim to align high sleep pressure with your circadian “sleep gate”.
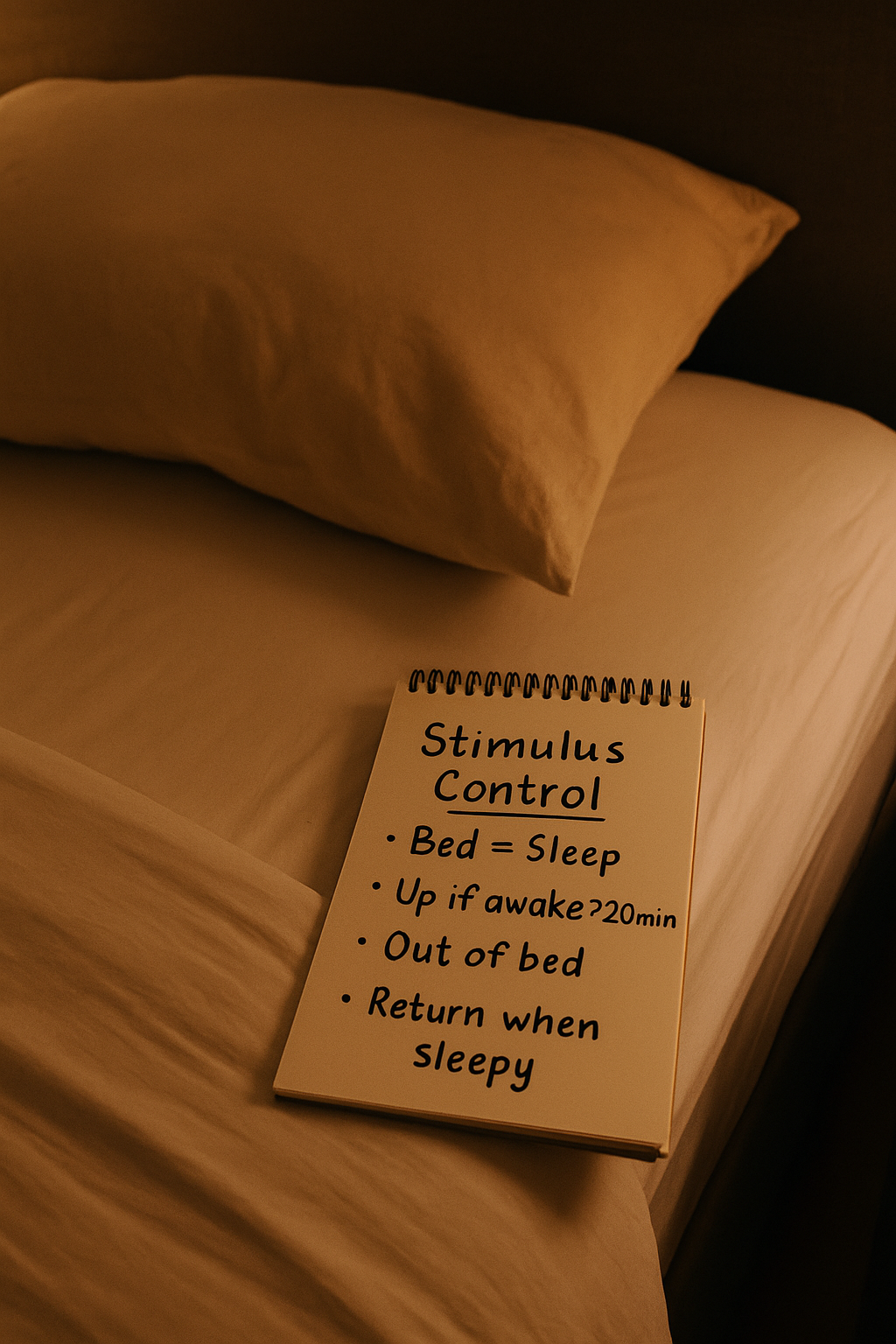
If you’re awake ~20 min, get up (dim light). Return only when sleepy.
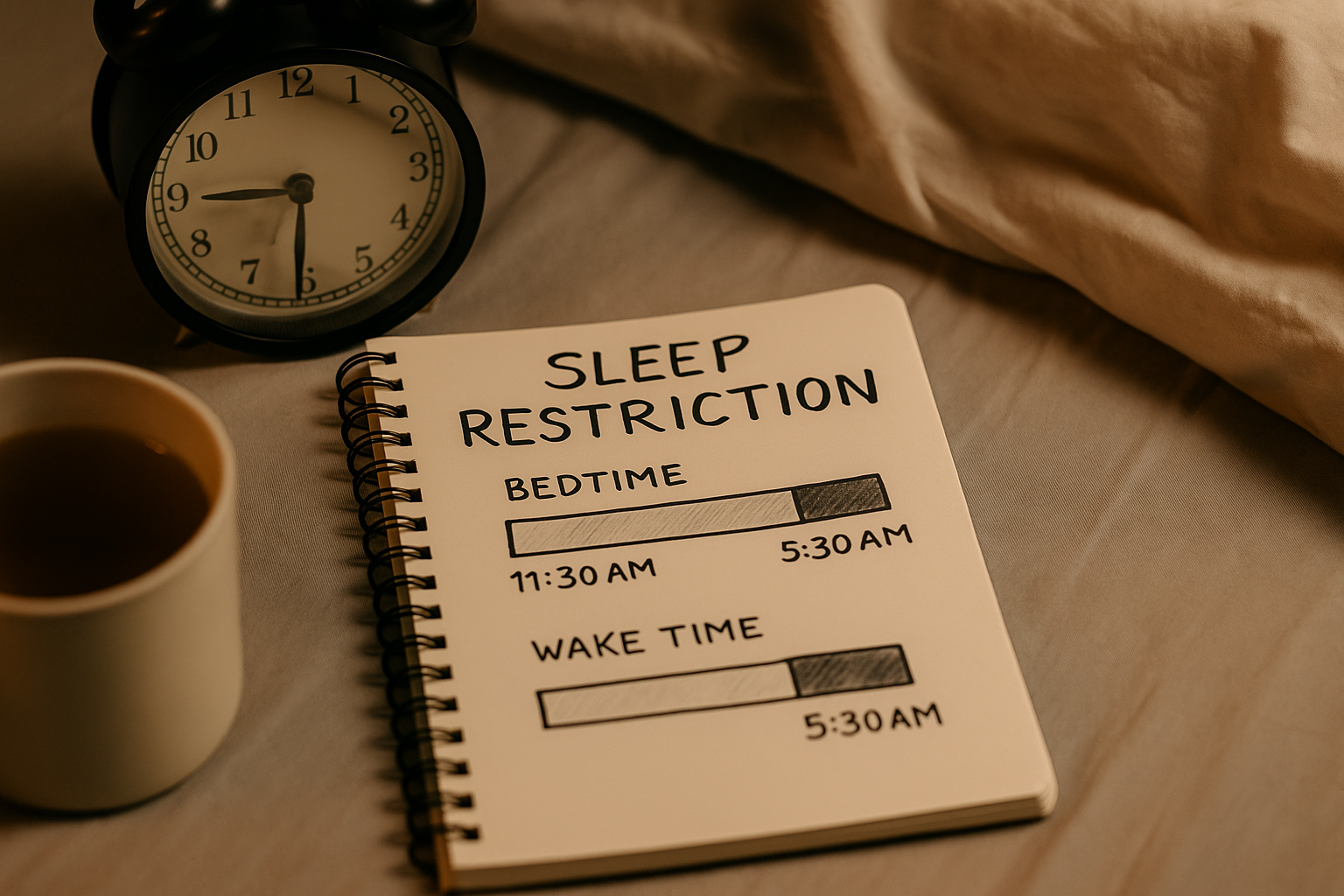
Match time in bed to actual sleep, then expand slowly.
Delayed clocks are biological. Work with it, nudge gently earlier.
The information on this page is for general understanding and support. It is not a substitute for professional medical or psychological advice. If you feel unable to keep yourself safe or someone else is at risk, call 999 (UK) immediately. If you’re outside the UK, contact your local emergency number.